Hopefully this answers some general questions for others. I will do my best to respond to comments at the end if you have any!
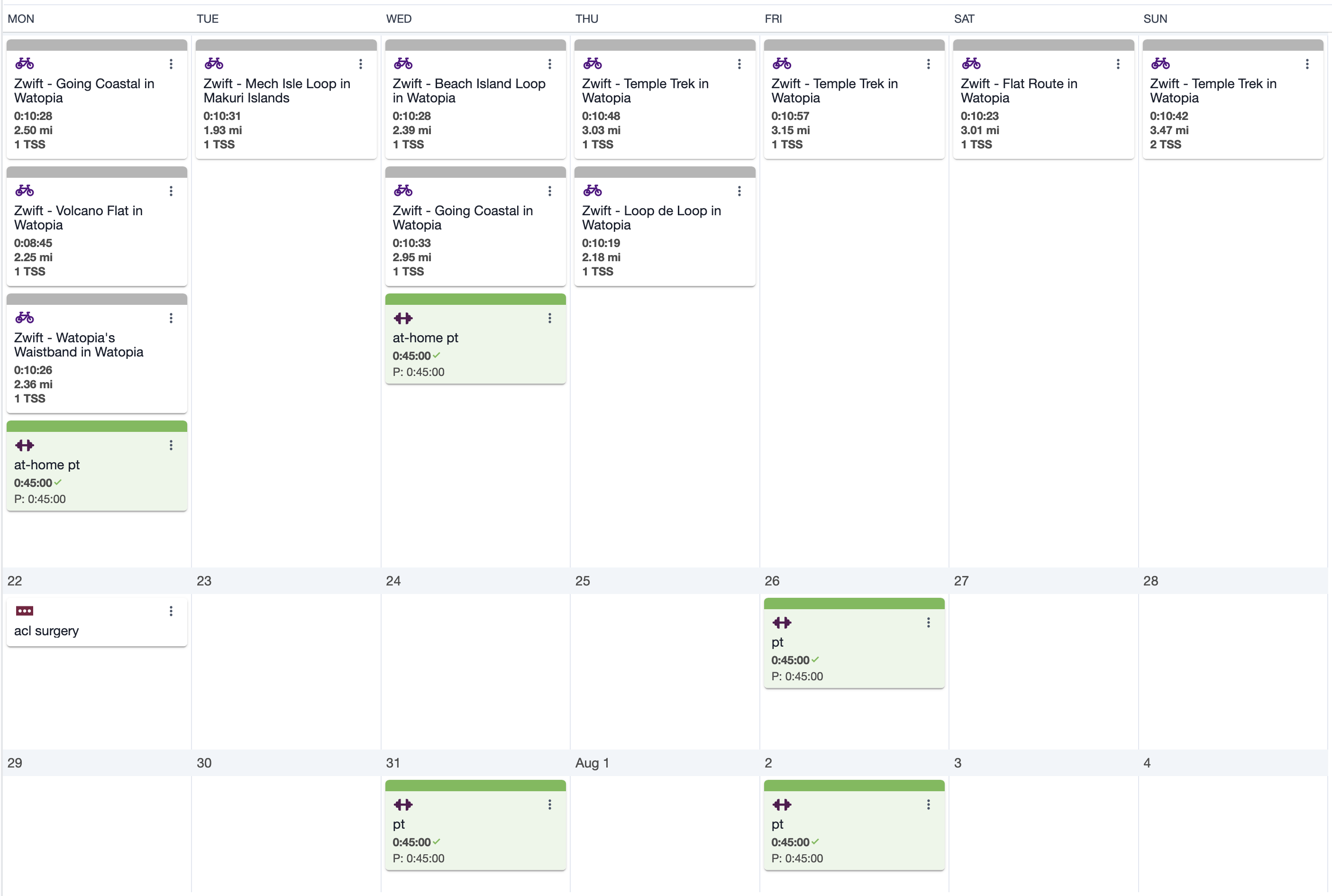
Phase 1: Post-Crash Prehab
On June 26, 2024, I was hit by a driver, and tore my right ACL, MCL, and broke bones in my left hand and right eye. I am an elite level cyclist (and only, no other sports) who had results at the top level of the sport in the US, so please take things in this post with that in mind. There is almost no research/recommendations for someone in my situation, so I wanted to share my timeline in a lot of detail. Please keep in mind that everyone’s timeline is different, and having the athletic background I do is a huge advantage. I would say this is the most accelerated approach possible.
For context, before my injury, I was capable of sustaining around 200+ watts during long rides. On my last pre-injury ride on June 26th, I averaged 201.68W with a weighted average power of 274W.
I spent a few days in the hospital after the crash, two of which were entirely immobile with me not moving or getting out of the bed. I then was discharged, and told to start at home PT ASAP to prepare for surgery. Because of the nature of the crash, the swelling across my whole body was pretty severe but the PT started off with massaging and basic mobility stuff. I was in a knee immobilizer so I could walk around the house, and had a walker set up to drag myself around. I was either in bed, on the pull out couch, or doing PT for the first few weeks.
PT started on 7/1, just 3 weeks before surgery and 5 days after the crash (3 days after being discharged) and was three times a week until surgery.
My main goal was getting back on the bike, which started just 1.5 weeks before surgery (two weeks after the crash) and when I got to ~90 degrees of flexion. Because of my MCL, it was extremely painful. It started out as 10 minutes of rock backs on flat pedals, basically pushing it as close as it would go (and I could tolerate) to a full rotation. Every pedal stroke felt like being stabbed on the inside of my knee, but I forced myself to do it. I limited the sessions to 10 minutes and stopped if things did not loosen up as time went on.
Two weeks after the crash I was able to do approx 50-80w with zero trainer resistance. I loaded Zwift up, but it was demoralizing barely riding 1 mile. The goal was to not lift my hip on every pedal stroke which was quite challenging but improved as my flexation increased. My cadence was 70-80 rpm by the end of the ride as things loosened up. The first few minutes were cry-inducing levels of pain to get things warmed up.
I quickly was able to increase the number of 10 min spins to twice per day, but 3 was too much. I was riding about 4-5 times weekly during this pre-surgery period, slowly building duration while keeping power low (averaging ~75 watts). My cadence during each spin gradually improved from the initial 55-60 rpm up to 70-75 rpm by the time I went in for surgery. There was a lot of listening to my body and being super conservative at this point. The goal was just to help increase flexion, not training.
After a few consultations with surgeons across the Colorado area, it became clear that the Steadman clinic was the only realistic option for me. My MCL tear was unique, so most surgeons said they wouldn’t be comfortable operating on me. Steadman’s aggressive approach to recovery and surgery aligned with me well, I knew my body would be able to take it pretty well.
Phase 2: Surgery + First Two Weeks Post-Op
Surgery was on 7/22, 3.5 weeks after the crash. I had my knee flexion up to 120 degrees, which was close to what the surgeon recommended. The surgery was fine, but the pain after mostly came from my calf below the knee. I have never experienced that much pain. Thankfully, it only lasted for 1-2hrs. Eventually was given the all clear to go home, and when I took my first step (with my brace) I immediately knew that the MCL was fixed.

I slept at home with a flat angled pillow, but it seemed to be hit or miss as to if it helped with the pain or not. The biggest struggle I had in the first week was pain wearing socks, the elastic band was causing the swelling to sit between my knee and calf which was no fun, would recommend getting some no-show socks with little to no elastic during this period.
I also got a CPM machine to use prior to starting PT, which helped tremendously. I only took the week after surgery off work, but was able to work from my couch with the CPM going after that. I was doing 2-3 hrs per day total in a few sessions, although I would later learn that my surgeon actually wanted 6+. I don’t think it had a major impact though, any amount is beneficial. I did my best to avoid pain killers, but there were some nights that I simply could not sleep without them. The brain fog was more limiting than the lack of sleep though so eventually I stopped taking them entirely.

I started PT at CU sports medicine 4 days post-op. I was still using the walker with an arm extension, since I couldn’t use crutches with my broken hand. Everything was reset from the previous prehab in terms of flexion and swelling, but things were a lot more normal without the MCL pain. We spent the majority of time focusing on straightening the knee, not bending it, as the first two weeks are essential for that.
My knee range of motion at this point was limited to 40 degrees, and I couldn’t perform a straight leg raise without a significant lag. We started with quad activation exercises using NMES (neuromuscular electrical stimulation) for 10 minutes and basic knee range of motion exercises.
PT Details from Early Post-Op Notes (Weeks 1-2)
At 4 days post-op my evaluation showed:
- Right Knee PROM: 10-40°
- Left Knee PROM: 0-135° (unaffected side)
- Wells Criteria: 0 (unlikely for DVT)
- Calf Girth Measurements (10 cm distal to tibial tuberosity): Right 33.0 cm, Left 30.0 cm
- Significant right knee effusion
- Initial LEFS score: 9/80
By 9 days post-op:
- Right Knee PROM improved to 3-64°
- Sweep Test: 3+ right knee
- Calf measurements: Right 31.0 cm, Left 30.0 cm
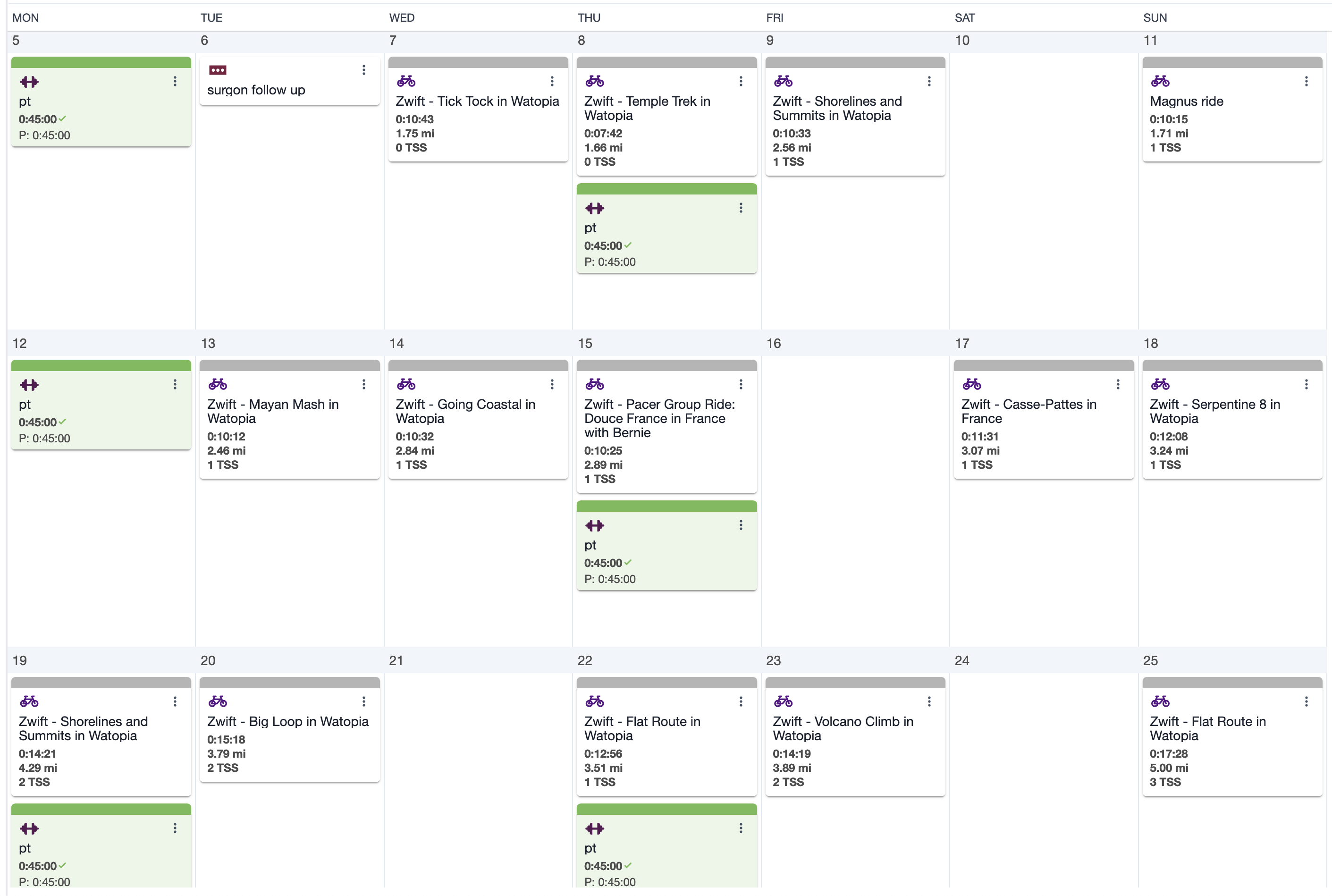
For the first two weeks post-op, I was doing PT exercises 5+ times per day. It was brutal, but I followed my PT’s directions exactly which prevented me from overdoing it and causing more issues. I was able to do full pedal strokes on 8/2, but limited it to rocking back and forth as I was still experiencing tension due to swelling and the bandages. I waited until after a follow up with the surgeon to ensure everything was okay before turning on Zwift with zero resistance.
On my first real Zwift session just over 2 weeks post-surgery, I was only able to maintain about 30-40 watts for 10 minutes with a cadence around 40 rpm. The power and duration were a significant step back from my pre-surgery rides, but mentally it was a huge win just to be back on the trainer. I rode these early sessions with my knee brace locked at about 30 degrees of flexion, which was uncomfortable but necessary for stability.
To manage swelling during these early trainer sessions, I used an ice vest which helped keep my core temperature down and reduced the post-ride inflammation. I’d freeze the ice packs overnight and put them in the vest right before getting on the trainer. This made a huge difference in how my knee felt both during and after rides.
At my two week follow up, the surgeon said everything was on track and my swelling was looking as expected. The focus was still on doing everything I could to reduce swelling. Over the following two weeks, it became clear that riding the trainer did not increase swelling the same way walking did, so my days turned into either being on the couch or trainer and not much in between. I kept the intensity low, but started to slowly increase the time on the trainer until I got the all clear at the 6 week mark from the surgeon.
One key discovery during this period was how effective the ice vest was for longer training sessions. As I started pushing beyond 20 minutes on the bike, I’d wear the ice vest for the entire session indoors. This cooling strategy, combined with elevating my leg immediately after riding, allowed me to increase duration faster than I initially thought possible. The vest became a crucial piece of my recovery toolkit that I hadn’t anticipated needing before surgery. Would recommend for sure to help with temperature regulation.
Phase 3: Weeks 3-6 Post-Op
During weeks 3-6, I continued to make solid progress. By week 3, I was able to ride at higher RPMs (around 80) without immediately needing ice afterward. I was visiting PT twice weekly, and we focused heavily on exercises like NMES for quad activation, straight leg raises, terminal knee extensions with resistance bands, and various mobility work.
At home, I used an ESTIM device to force my quad to activate. This was incredibly beneficial in retraining my brain to activate my quad muscle, but at some point it stopped being as effective.
Cycling Progression (Weeks 3-6)
Here’s how my riding progressed:
| Week Post-Op | Avg Duration | Avg Power | Cadence | Daily Distance | Brace Status |
|---|---|---|---|---|---|
| Week 3 | 10-15 min | 30-40W | 40 rpm | 2-3 miles | Locked at 30° |
| Week 4 | 20-25 min | 55-70W | 60-70 rpm | 3-4 miles | Unlocked, limited ROM |
| Week 5 | 25-30 min | 80-110W | 70-85 rpm | 3.5-4.5 miles | Unlocked |
| Week 6 | 25-30 min | 130-150W | 85-90 rpm | 4-5 miles | No brace |
I was progressing from single-digit Zwift rides at the beginning to rides of 4-5 miles by Week 6, with consistent improvements in both duration and power. Throughout this period, I continued using the ice vest during most rides, which helped manage swelling especially as the duration increased. By week 5, I found that the combination of the ice vest and a post-ride elevation session was optimal for recovery.
Walking was still challenging. I progressed from using the walker to a cane with my brace locked, though due to my left hand fracture, I had to use the cane on the same side as my injured knee. My PT introduced blood flow restriction (BFR) training around week 5, which was uncomfortable but effective for building strength without stressing the joint. We were also working on step-downs from small heights (2-4”) and practicing gait patterns.
By this point, I was no longer wearing the knee brace during trainer sessions, which made a massive difference in comfort and output. Around week 5, I experimented with short rides without the ice vest and found that as long as I kept cadence high (85+ rpm) and resistance low, I could manage 25-30 minutes without significant swelling response. However, for any higher intensity work or longer sessions, the ice vest remained essential.
By 4 weeks post-op, my knee range of motion had improved to 100 degrees, though I still had a 3-degree lag during straight leg raises. By 5 weeks post-op, I had no lag during straight leg raises, and my knee flexion had improved further to 112 degrees.
Emotionally, it was a rollercoaster - some days I felt great progress, while others were frustrating with lingering swelling and discomfort, especially when I’d been more active. My calf and knee would often feel tight and achy after standing too long.
At 5 weeks post-op, I started riding with erg mode. I was able to do 160w for the “on” part of that ride, and it was a bit ambitious and caused a lot of joint discomfort but felt like a huge step in my recovery. I was set on being able to increase power and training load after the 6 week mark.
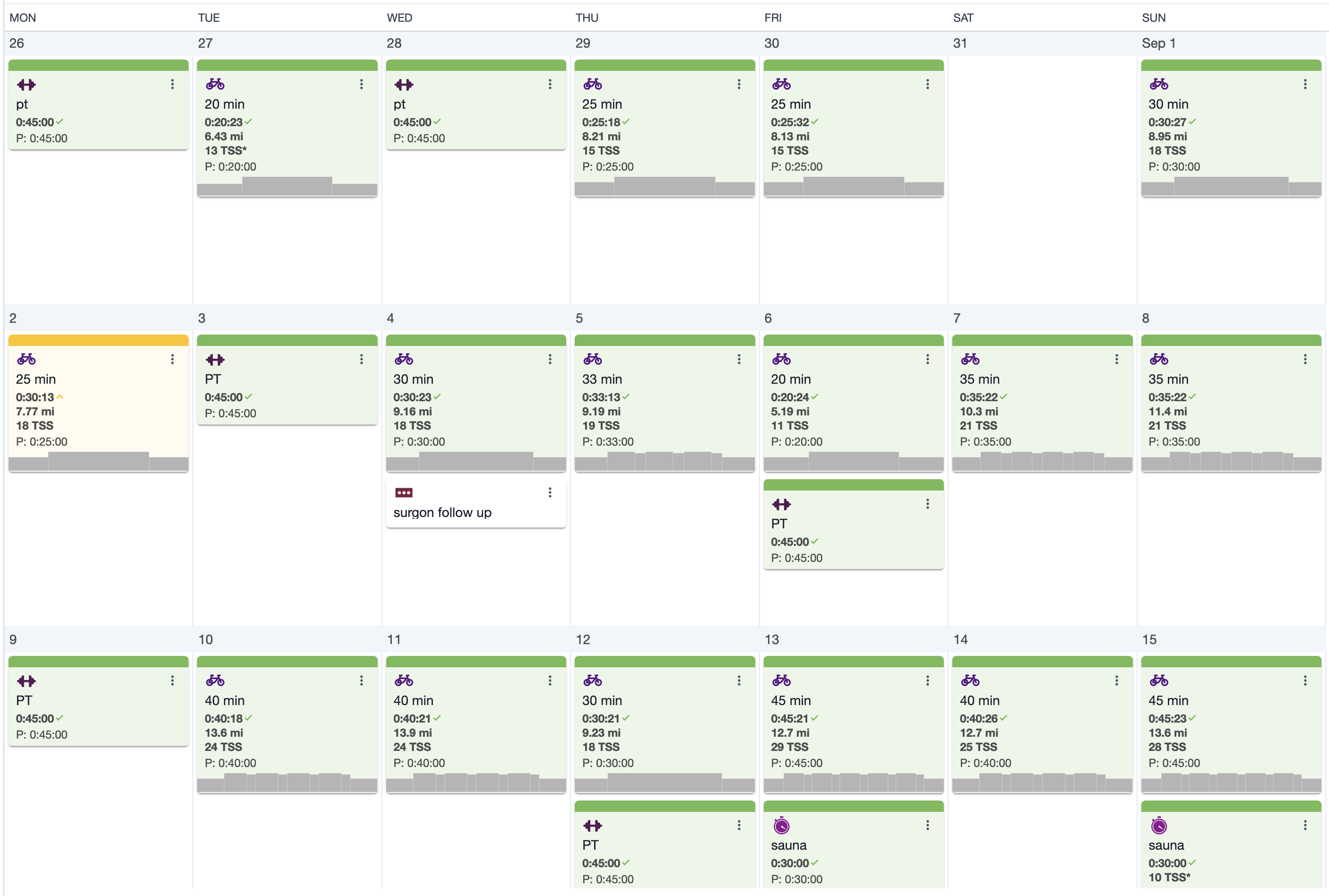
Phase 4: Weeks 6-12 Post-Op
I met with the surgeon for the 6 week follow up. I knew my progress was going well, but the surgeon said I was doing exceptionally well with swelling considering the MCL. The disappointing news was that I would need to wait until the 12 week mark until I could really ramp up the training. I did get the all clear to use the sauna post ride, so that helped me with feeling like I was getting more cardio load without increasing duration on the bike.
I was told to only increase training volume in 10% increments every few days, and I followed that religiously. I never missed a ride and was able to have a linear increase on my weekly/daily volume almost perfectly.
Cycling Progression (Weeks 6-12)
The progression during this period was remarkable:
| Week Post-Op | Avg Duration | Avg Power | Cadence | Weekly Vol |
|---|---|---|---|---|
| Week 6 | 30 min | 130-150W | 85-90 | 2-3 hrs |
| Week 7-8 | 45 min | 150-170W | 85-90 | 5-6 hrs |
| Week 9-10 | 60 min | 170-190W | 85-95 | 10-12 hrs |
| Week 11-12 | 70 min | 180-200W | 90-95 | 15-20 hrs |
By week 9, I was hitting 45-50 minute rides with higher intensities. I was finally given clearance to ride outside with clips after my 3-month surgeon follow-up, which was a major milestone I had been eagerly awaiting.
During weeks 6-12, I continued PT 1-2 times weekly. My exercises progressed to include more challenging movements. We did a lot of manual therapy for my patellofemoral joint mobility and scar tissue, combined BFR training with leg press and knee extension exercises, and added functional movements like wall sits and step downs. We also used the GTS (Gravity Training System) for controlled squats and hamstring work.
Around weeks 9-10 post-op, I started experiencing sharp pain in my shin when standing up after sitting, which my PT felt was related to swelling and tissue irritation. We addressed this with soft tissue massage and modified activities. My walking was improving, and we began practicing without the brace but still with the cane.
By Week 10, I was able to do partial range knee extensions with 15 pounds and leg press with 120 pounds on my surgical leg (compared to 160 pounds on my uninvolved side).
At my 10-week mark, baseline strength testing showed my right quadriceps were at 65.2% of my left side strength. My rate of force development was also 77% slower on the involved side. During the 1-minute single leg squat test, I managed 11 reps on my surgical leg versus 23 on my uninvolved side. Despite these deficits, my cycling was progressing well, with my power numbers continuing to climb week by week.
Knee effusion (swelling) was gradually decreasing, though still present. My knee was responding better to activity, with less swelling and faster recovery between workouts. We also started working on hip hinge movements to improve my functional biomechanics.
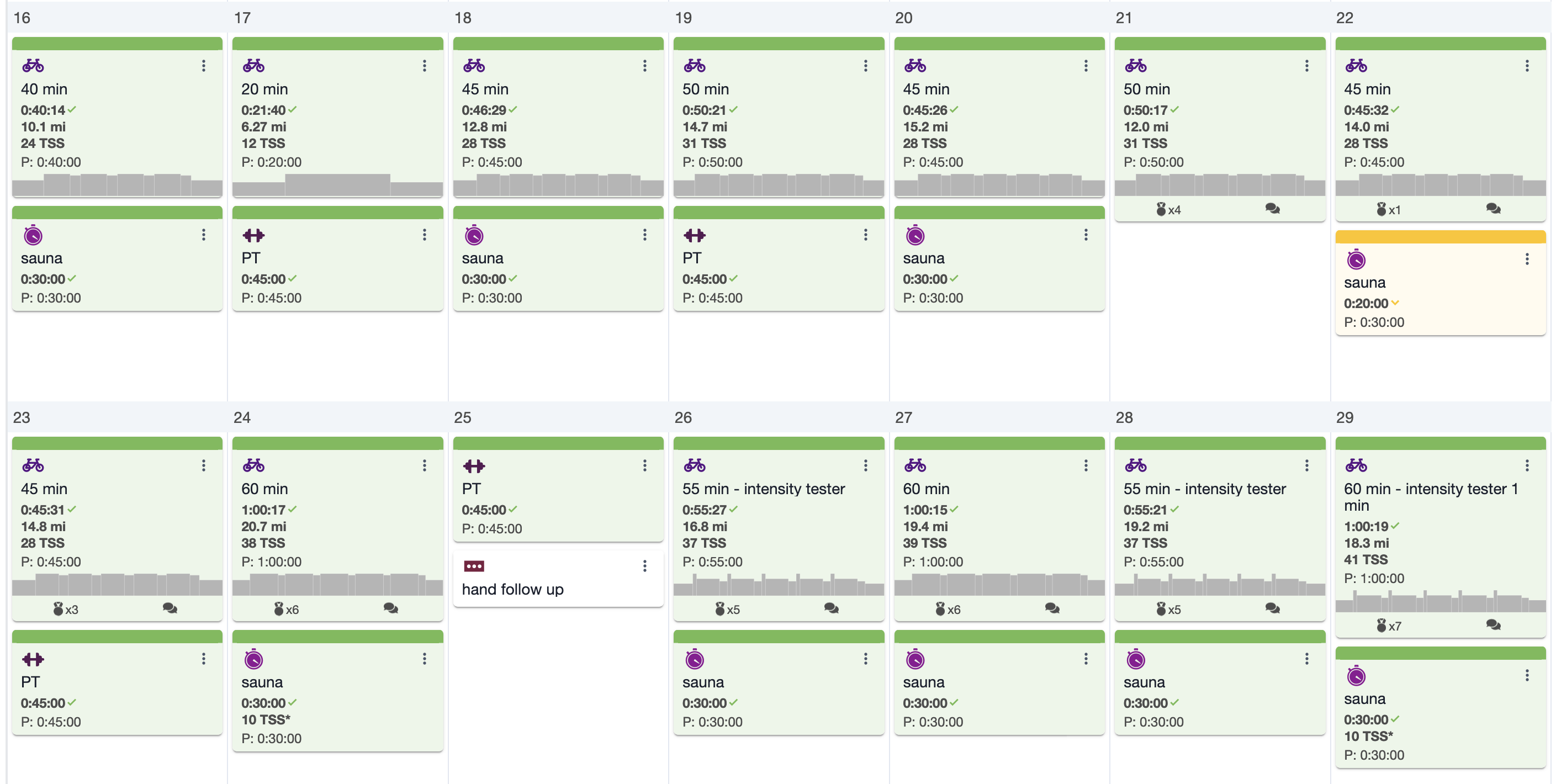
Phase 5: Months 3-4, Riding Outside
By the 3-month mark, I was finally allowed to properly ramp up training intensity. During this period, my PT sessions included more advanced techniques like trigger point dry needling for my vastus lateralis, rectus femoris, and other muscles that were contributing to lingering discomfort. These sessions were uncomfortable but made a huge difference in how my knee felt afterward.
First Outdoor Rides

I completed my first outdoor ride at 3 months post-op (Oct 26), covering 50 miles on a gravel bike. I averaged 87.79W with a weighted average power of 118W. The next day I rode again for 48 miles at similar power. These outdoor rides were a significant mental milestone, even though my power output was still well below my pre-injury levels.
I took a 10-day trip to Girona to ride at around 14 weeks post-op, and in retrospect it was a bit too early. During this period (early November), I was doing rides of 20-60 miles with average powers between 60-130W, significantly below my pre-injury capacity. When riding with others, I would get gapped pretty dramatically at stop lights since I didn’t have the muscle strength to accelerate. I did the trip at ~14 weeks, but would have probably been much better off delaying it another few weeks. But it was a good goal that brought me through the earlier stages of recovery so it served its purpose in that respect.
My PT and at-home exercise program expanded to include more complex movements - lateral step-downs, eccentric calf raises, band work in multiple directions, and various balance exercises. I was starting to feel like an athlete again rather than just a patient. I continued this routine even when in Girona.
LA Training Trip
In November (around 4 months post-op), I took a big step forward with a training trip to LA where I completed three consecutive long days: 2.5 hours, then over 6 hours (with 12,000 ft of climbing), and 5 hours on the last day. I was nervous about how my knee would handle it, but it responded better than expected.
My power output was nearly back to pre-injury levels except for the final day, with my left side still producing 5-10% more power on average. My confidence on descents was returning too, which was huge mentally. Monitoring left/right balance was helpful, but only in the sense that I could see a difference when I focused on producing more power on my injured side.
After the LA trip, I felt fatigued but not as much as expected - my knee had some stiffness but no major setbacks. By December (around 5 months post-op), I was up to around 20 hours of weekly training volume and handling significant elevation gain. I still noticed my right leg felt different, especially when starting from a stop, but it was improving weekly. I transitioned to doing PT about once a week at month 4, focusing on strengthening and neuromuscular control exercises like Copenhagen holds and single-leg movements.
Phase 6: Months 5-8, Returning to Competition
At 6 months post-op, my quad strength had improved to about 80% of my uninjured side according to testing at Steadman, and I was gradually increasing my outdoor riding with only occasional stiffness. My PT sessions focused on improving that remaining quad weakness through dynamic exercises and continuing blood flow restriction training.
By this point I was making impressive progress - riding 7+ hours sessions and completing 100+ mile rides with close to normal power outputs (220-240 watts average). My cycling volume was back to 20+ hours weekly.
Strength Progress At Month 6-7
By January 2025 (around 6 months post-op), my strength metrics showed:
- Quadriceps strength symmetry: ~80% of uninjured side
- Right quadriceps circumference: 45.5cm compared to 48cm on left thigh
- Single-leg press: 120 lbs on right leg versus 160 lbs on left
- Left/right power balance on the bike: improved to 53% left/47% right
I was doing a lot of single leg press (up to 120 lbs on my right leg versus 160 lbs on the left), neuromuscular re-education with cable rotations for trunk control, and more challenging balance work.
At 7 months post-op, I was consistently training at high volumes (20+ hours weekly) with good recovery. One weekend included 14,000ft of elevation gain, which left me with whole body fatigue but minimal knee issues. My PT was using dry needling to help with lingering tension in my knee and muscles, which was making a noticeable difference. We were targeting TFL, vastus lateralis, and calf muscles primarily, as these seemed to be compensating in ways that affected my knee.
I noticed that when I didn’t ride, my knee actually felt worse - movement seemed to help it feel better. I was doing a lot of single leg exercises, including some early plyometric prep work and band-assisted speed lunges to prepare for more dynamic movements.
Power Data Return to Competition
Here’s the progression to near pre-injury levels:
| Month | Avg Ride Duration | Avg Power | Weekly Volume |
|---|---|---|---|
| Month 3 | 1-2 hours | 90-120W | 8-10 hours |
| Month 4 | 2-3 hours | 130-170W | 12-15 hours |
| Month 5 | 3-4 hours | 170-200W | 15-18 hours |
| Month 6 | 3-5 hours | 190-220W | 18-20 hours |
| Month 7 | 4-6 hours | 210-230W | 20+ hours |
| Month 8 | 5-7 hours | 220-240W | 20-25 hours |
By February-March 2025 (7-8 months post-op) I was completing multi-day blocks with impressive numbers:
- Feb 20-22: Three consecutive days with 120-180 mile rides, averaging 230-240W
- Mar 7-9: Three-day block with nearly 190 miles on the final day, averaging 218-235W
At 8 months post-op, I was riding Flagstaff Mountain with minimal complaints - a huge milestone considering where I started. My LEFS (Lower Extremity Functional Scale) score had improved from 9/80 initially to 49/80, showing significant functional progress. I was still feeling some medial knee discomfort that we addressed with instrument-assisted soft tissue mobilization (IASTM), which seemed to help.
I still tended to reduce right knee flexion during certain exercises, and we were working on assisted plyometric variations to improve this. We incorporated banded exercises to add more quadriceps and hamstring strength in functional patterns.
Riding finally felt normal again, though I still notice my knee feels best when I’m riding regularly. The recovery journey has been long and challenging, but the consistent progress throughout has been rewarding. Being able to return to high-level cycling competition makes all the hard work worth it.
Final Thoughts
This journey has been challenging but incredibly rewarding. I’m grateful for the systematic approach my PT team took, especially in balancing my desire to return to high-level cycling with the need to rehabilitate properly. For anyone going through a similar injury, I’d emphasize a few key lessons:
- Consistency matters more than intensity, especially early on
- Follow your PT’s guidance, but also be your own advocate
- Track your progress meticulously - it helps during those frustrating plateaus
- Be patient with strength asymmetries - they take time to resolve
- Find the right balance between pushing forward and allowing proper recovery
The most important factor was having clear communication with both my surgeon and PT about my specific goals as a cyclist, which allowed us to tailor the rehabilitation approach to my needs while still following evidence-based protocols for ACL and MCL recovery.
Nine months post-surgery, I’m back to competitive cycling with minimal limitations - an outcome I wasn’t sure was possible in those first painful weeks. If you’re going through something similar, stay positive and trust the process - it works!



Comments